
Some medical practices may want the fully-written SOAP note to be reviewed and/or approved by a higher-up, while some practices will want the SOAP note writer to upload the completed document to a database of medical records. The next steps, just like the plan itself, will differ. Additional/extra tests that should be conducted.Referrals to other medical departments or personnel.Every plan written for each patient will be entirely situational depending on who they are, what the issue is, and what stage they’re at, but plans often include: It’s here that I’ll create a post-session plan. The fourth and final component is the plan component. I’ll also write a note here regarding how your state has improved or worsened since your last visit. Regarding the last point, let’s, for instance, say this is your second visit to the practice regarding the issue but your first visit to me as a physician. And relevant information concerning progress.And the results from laboratory and diagnostic exams.Īfter that, it’s time to write notes related to assessment.Vital signs and measurements, such as blood pressure and weight.When writing the objective section, I’ll make to sure write down: Plus, I’ll be writing up any findings of any examinations and tests that you’ve had done. Here, I’ll be writing information on what I’ve observed from what you, the patient, are physically displaying and what you’ve verbally told me during our meeting. Once those basics are out the way, I can then move onto the objective component of the SOAP note. Where the chief complaint is located in the body.

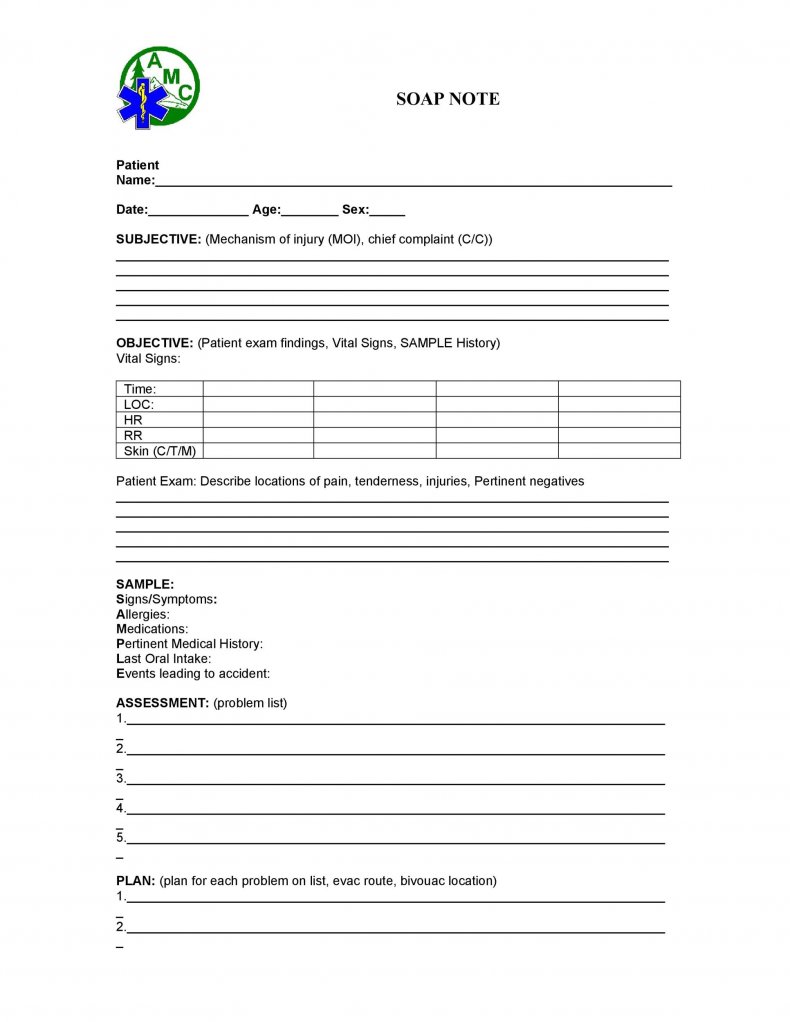
The CC, otherwise known as chief complaint (which, in this case, is the arm swelling).Although each component will differ depending on the patient and at which stage the note is being written (numerous notes are written at differing points until the issue is fully rectified), the subjective component often includes information such as: The physician (me) attended you and I now need to write an initial document that follows the SOAP structure.įirst, I’ll be writing the subjective component. To illustrate how a SOAP note works, let’s roleplay.Ī patient (you) came into a medical practice with arm swelling, but no diagnosis or idea what the issue at hand could be. To see what a SOAP note template looks like, check out (and use!) this example from Process Street:Ĭlick here to get the SOAP Note Template! How does a SOAP note work? SOAP notes, once written, are most commonly found in a patient’s chart or electronic medical records. SOAP notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. So what’s up, Doc? Ready to get reading? 👀Ī SOAP ( subjective, objective, assessment, plan) note is a method of documentation used specifically by healthcare providers. Using Process Street for your SOAP notes (and more)!.Read through the below sections to get clued-up: To boot, I’ll also show you how Process Street makes writing and implementing SOAP notes extremely easy. In this short yet informative post, I’ll explain what a SOAP note is, its interesting history, why it’s useful, and provide a visual example of what a SOAP note looks like. ( Spoiler: It’s not related to the cleaning product.) To help make this near-impossible task a reality, many healthcare providers turn to what’s known as a SOAP note. Healthcare providers, then, need to strike the fine balance of providing each patient with adequate care but within an appropriate timeframe. However, even before the novel coronavirus struck, those working in the healthcare sector were run off their feet – especially considering there are only 2.6 doctors per 1,000 patients in the United States. It’s through their hard work, diligence, and courageousness that we’re able to recover from injuries and illnesses alike. Healthcare providers are the backbone of humanity.


 0 kommentar(er)
0 kommentar(er)
